
*Original post released on 9/30/2020
The Intensive Care Unit (ICU) can be an intimidating place for the new nurse, the nurse switching from a different specialty, or really any nurse. The ICU is a constantly changing environment with patients that demand an incredibly rigorous level of care. Walking onto the unit, each day is different and things can change in an instant. Aside from preparing yourself academically for the rigors of this setting, there are a few tips and tricks many of us pick up along the way that help ease the stress of this environment. In this article, I want to share with you the pointers I’ve learned during my career as a critical care registered nurse. First, we’ll start off with some general tips and tricks. This will be followed by a few tips for before, during, and after your shift. Let’s get started!
General Tips & Tricks

Whenever you are new to a unit or facility, it’s always a good idea to know where key equipment and supplies are located. Examples of such equipment and supplies would be the crash cart (imperative for ICU nursing staff), IV pumps, beds, assistive/transportation equipment, medication room, respiratory therapy (RT) equipment, hemodynamic monitors, oxygen tanks, dopplers, rapid sequence intubation (RSI) boxes, and intubation trays. Along with this, it is important to note where other emergency equipment is located (Ex: fire extinguishers, AEDs for times of transport throughout the facility, etc.). Be sure to know your facility’s protocol for various emergency events and how this applies to patient care.

Invest in a solid (and current) ICU resource book to keep in your locker at work to have on hand for reference. I know there are many online services, such as Clinical Pharmacology or Up To Date, that offer information at the tips of your fingers at a moment’s notice; however, to me, there’s nothing like having a great quality physical book as a resource. A commonly used reference book for many ICU nurses is “The ICU Book” by Paul Marino. This book has both a full version, which is pretty large, and a pocket version. Amazon has both versions available for rent or purchase (full – $42 rent/$88 buy; pocket – $18 rent/$36 buy). I do believe someone on another site has a PDF version of the full size ICU book online, which I’ll link HERE while it’s still available. Be sure to check it out.

After working for a few months on nights with one of my favorite charge nurses, I noticed that she would carry around a pocket book that contained the phone numbers (both office and personal) for the physicians that interacted with our unit. I remember always having to ask her for phone numbers when I would have to call a physician in the middle of the night, and often times the hospital directory numbers offered delayed responses at best while hers did not. My tip here? GET ONE! It can be an invaluable resource to have, even if (at the bare minimum) it stays in your locker until needed. You may not always have your phone on your person, so if you get in the habit of keeping this in your pocket, physicians are literally a moment away. A key example of when this may be an invaluable resource is during a rapid response to the floor. ICU nurses are often assigned code duty for the facility, meaning that if a patient’s condition deteriorates while they’re on a medical floor, they’re the ones evaluating the patient’s status to determine if higher level of care is required. These tend to occur at a moment’s notice, so having this book in your pocket can reduce delays in communication. This is the one I use (available on Amazon).
As you start to get comfortable in your role as an ICU nurse for your facility, I suggest considering working your three shifts in a row. This can be tiring, yes, however there are multiple benefits to doing this as well. Not only will working your shifts in a row help maintain consistency and continuity of care for your patients, it can also help you see the progression of their care over time as well as the return on the investment of your time and effort in their care. This can help build and establish enhanced rapport and relationship with your clients. Furthermore, picking up extra shifts when help is needed shows your team and managers devotion to the job and your unit, teamwork, and helps keep you in the forefront of their mind for new learning/training opportunities.
Be sure to make friends with your coworkers as they are your largest support system both on and off shift, especially if your family members, significant other, and friends are not health care professionals (HCPs). Moreover, cultivating good relationships within your team helps to foster teamwork and develop the unit as a whole. Keep in mind that work is lighter with more hands. Work smarter, not harder. Many times at night, I’ll offer to help the nurse with patients next to me during their bed baths and linen changes for exchange in helping with mine. This makes for easier and faster completion of tasks for both parties.

On a different note, something I’ve recently discovered myself is the awesomeness of the nursing utility belt (AKA: the nurse “fanny pack”). I was incredibly skeptical at first and wasn’t overly ecstatic about using a fanny pack; however, I am now a BIG advocate of them! Just think about it, seriously… Using a utility belt helps reduce the waste of supplies because items are not left in the patient’s room/drawers when not needed. Moreover, you’re always prepared no matter where you are or what the situation is (again, consider a code or rapid response situation). Along with this utility belt, I strongly advise considering the use of a stethoscope holder for your belt or the waistline of your scrubs. It secures your stethoscope on your person at all times, which not only keeps you prepared for a focused assessment at a moment’s notice but also *hopefully* deters theft.
Finally, make sure you’re seeking out learning opportunities whenever possible! Go on code duty even if you’re not assigned that day, or even if you’re still on orientation status. Pursue any available training opportunities and continuing education courses (Ex: ACLS, PALS, TNCC, CCRN, etc.). Be sure to see what your facility will pay or reimburse for, but don’t let this deter you from seeking out higher learning opportunities that may not be covered. If it improves your level of knowledge and competency, IT IS what’s best for your patient in the end (aside from simultaneously advancing your own career). If an experienced nurse has any advanced or unfamiliar equipment or patient cases (Ex: EKOS, IABP, Impella, CPT, wound vacs, open surgical patients, vents/trachs, etc.), have them teach you about it! Please make sure to be courteous and considerate when approaching these nurses for a teaching session by making sure they have a free moment to do so. Or, even better, offer to help them and discuss the case/equipment as you assist them!
Shift Tips & Tricks

Now let’s move on to your actual shift itself! Before you start any shift, be sure to come to the unit prepared and early (approximately 15 min early is a good timeframe). Most facilities will allow you to arrive 15 min early. At the minimum, make sure you have your stethoscope, a pen light, 2 pens, 1 pencil, trauma shears, hemostats, a clipboard, and your nurse utility belt if you have one. Consider using a stethoscope case or pencil pouch for easy storage and grab-and-go of all your gear. Furthermore, if you have any pocket resources, make sure you have them on hand for when other nurses or professionals cannot be present to assist you or answer your questions. I offer a few pocket resources in my Etsy shop that I personally use in the ICU setting: ICU IV drip cards, ECG Interpretation cards, critical care ID badge cards.
If it’s your second or third shift, I recommend quickly reading up on your patient’s most recent progress notes and check for any new changes to their orders. If it’s your first shift of the week and a new patient assignment, read up on your patients as much and as early as possible during the shift to provide you with a more complete picture of their health status as well as the provider’s approach to their care and treatment. This action also helps improve the continuity of care. Continuity of care for the patient is not a passive process; it requires effort on your part as well. It is not simply achieved by having the same patient assignment for three shifts in a row.
At the beginning of each shift, after receiving report, make sure you check on your patients and set the monitor’s alarm parameters. This is made incredibly easier by having BEDSIDE shift report. In the end, you are liable for the patients you assume care for and seeing those patients, WITH the off-going nurse present, helps maintain accountability and prevents you from assuming care of an unstable patient/situation. I also recommend assessing alterations in skin integrity and any wounds together before the off-going nurse leaves. Then, check all your IV pumps to see what’s infusing and double check the rates and doses against the order on the patient’s E-Mar. Verify for accuracy prior to the previous nurse leaving! Then, set your alarm parameters based on what’s infusing. In general, my typical monitor alarm parameters are: HR 59-110, RR 8-29, SBP 85-160, DBP 60-110, MAP 65-100, O2 sat 88-100.
Now that you’ve taken report and the previous nurse has left, my next susggetion at this point is to take a few minutes to review each patient’s medications and recent lab results. Knowing the timing of their medications as well as what medications are available to you as needed (PRN) arms you with invaluable information. Trust me on this, you DO NOT want to be the nurse who gets into an unstable hemodynamic situation and doesn’t know what PRNs are at their disposal to help the patient and likely stabilize the situation. Plus, knowing this information will help prevent you from making an unnecessary phone call to the provider at 2 am in the morning, which will likely be followed by a scolding. Additionally, it is important to know the patient’s most recent laboratory results as they pertain to their scheduled medications. Many critical care meds are either really or hepatically dosed and require you to be aware of this so patients receive competent care.

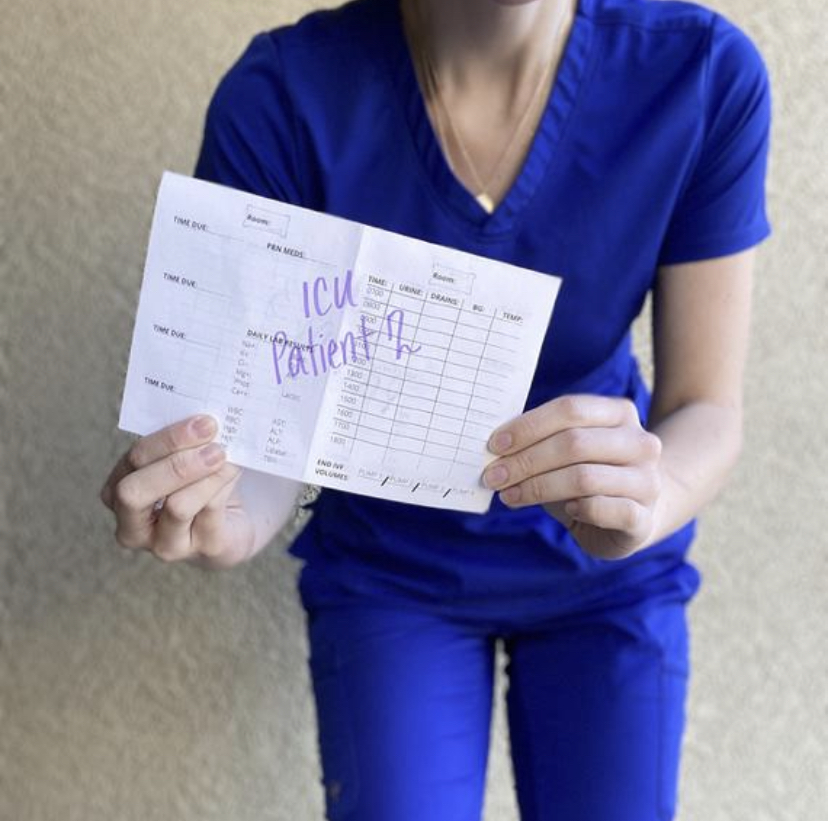
During your shift, it is imperative in this setting to stay organized throughout those 12 hours. This is accomplished by knowing the patient’s medication schedule, any pending studies/procedures, which physicians or specialties are visiting, etc. Using a pocket organizer for your patients and/or a vitals sheet can help you keep track of these and so much more! Want a tip for managing all those drips? Place a label on the line just above the y-site AND on the pump itself. This makes each line and medication easily identifiable in an emergency situation which helps reduce likelihood of errors. Then, tape a tongue depressor to the curve on the upper bed rail nearest to the pump and run the IV lines behind this to prevent accidental pulling/disconnection. The photo to the right demonstrates this tip, however they are using a medicine cup taped to the bed rail instead. Also, I personally would have untangled those lines in the photo a bit better than they did.

When it comes to bathing and linen changes, there are a couple of tips that are handy to have in your arsenal. For instance, I always like to keep all of my bathing/hygiene items in a drawer separate from any IV or medication supplies left in the patient’s room. In my mind, this substantially helps reduce risk of contamination and infection transmission. Make a bed roll ahead of time whenever possible. This can be done by using an empty or vacant bed…put all side rails up, place the fitted sheet over the rails, spread out your draw sheet, place your chux as desired, roll up from left to right (or vice versa). The photo to the left shows a bed roll being actively used. This will save you time and help improve your patient’s overall comfort. Speaking of this, be sure to pre-medicate your patients prior to any painful actions or procedures to enhance their comfort (Ex: prior to wound care, transfers, CPT, etc.). This is an example of using your PRN medications wisely!
Finally, after your shift, it is truly important to allow yourself to decompress afterwards (using healthy methods of course). I suggest having an “unwind” and bedtime routine, especially once you’ve started your stretch of shifts, to maintain consistency and maximize recovery. Don’t neglect your self care and feelings, because you cannot pour from an empty cup. To effectively take care of your clients, you need to care for yourself first. If you’ve had a particularly rough shift, a traumatic code, or experienced some other major situation, consider finding a person you trust to serve as a confidant. Alternatively, you can also seek out employee counseling for these same circumstances as your employer likely offers these as a free service to its employees. If help is available to you at no cost, please use it. Working in a critical care area such as the ICU, ER, OR, etc. can be mentally, physically, and emotionally taxing on anyone over time. It is perfectly okay to talk to someone who will be able to understand what you’ve experienced and is trained to help you manage the situation; this is also why family members may not make the best confidants.
I really hope these pointers provide you with some new information to help you learn, work, and care for patients more efficiently in the critical care setting. If you have any other tips and tricks of the trade that you’ve developed or learned over time, share them below in the comments to help each other out! I’d love to hear what you all have to say. Until next time, happy studying!
XOXO,
Andra Alyse

