*Original post released on 5/28/2023
You may be a nursing student or new grad nurse wondering how on earth seasoned nurses seem to be able to anticipate an impending code blue. It is possible for you to learn to see the warning signs too, which can ultimately help save your patient’s life. In this article, we’ll discuss a couple of major points to keep in mind when making the judgment to call for a rapid response team. Then, we’ll discuss some of the subjective and objective signs and symptoms that can reveal to you a code may occur.
Many of the patients at higher risk for a code situation reside on units that implement less monitoring, such as medical-surgical units. While the patient’s acuity may be higher on telemetry and critical care units, often times, subtle changes go undetected in a timely manner on units with less frequent monitoring. Typically, the patient at risk for a code will begin to exhibit signs and symptoms as early as 24 hours prior to the code situation. It is our job as nurses to collect subjective and objective data, interpret that data, and apply it to the situation to determine the best course of action for that patient.
Subjective data are those markers expressed by the patient, their family, and/or the nurse that are not typically measurable or quantifiable. For example, maybe the patient has expressed concerns about their state of health or have stated that they don’t “feel well.” In your own observations, you may make the judgment call that the patient doesn’t “look well.” Your patient and their family are the most reliable point of reference concerning the patient’s subjective status in light of whatever objective data you are able to collect.
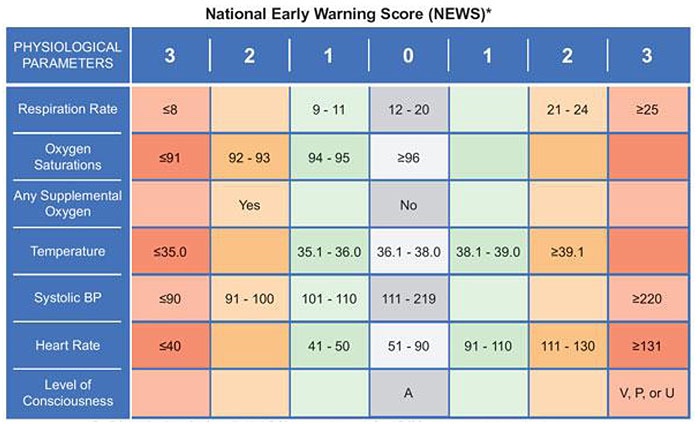
Conversely, objective data are those markers that are directly measurable or quantifiable. A great example of this is a patient’s vital signs. There is a scoring tool called the “National Early Warning Score” or NEWS score which rates the patient on a scale of 0 to 24 based on their vital signs, mental status, and urine output. When a patient scores higher than a 4 out of 24, it is time to consider calling a rapid response team or RRT.
Other points of objective data collection include assessing the ABCs (airway, breathing, circulation), mentation, pain, GI, and GU status of the patient. Is the patient able to maintain their airway and keep it clear and protected? Are they breathing too slow, fast, or not at all? Are they able to talk normally? Are they requiring higher oxygen demands in light of their shortness of breath? How are the pulses, color, and temperature of their extremities? What’s their level of consciousness like? Do they have altered mental status? New onset lethargy? Are they agitated, restless, uncoordinated, or have alterations in their speech? Is their pain new? Has it changed in intensity or character/quality? Is the pain accompanied by other symptoms as well? Is their new or an increased amount of discharge from a wound? Has the patient started to bleed or have increased amount of bleeding? Are there more frequent arrhythmias, chest pain, abdominal distension, etc.?
All of the aspects in the previous paragraph are simple areas in which to assess your patient to help you evaluate if their state of health is deteriorating (and possibly help assess the intensity at which their health is deteriorating). The key to getting ahead of these problems and treating them before they do irreparable damage to your patient is to recognize many of those early warning signs BEFORE they’ve progressed to a point of organ damage or worse. The nurse is the person who spends the majority of time with patients while they’re admitted. It is for this reason that healthcare providers rely on us to recognize, escalate, and intervene when multiple warning signs are present.
I hope this article helped you see the many different points you can easily include in your assessment routine to help you think critically and intervene when necessary for the sake of your patient’s health. You don’t have to be a “seasoned nurse” to have a sense that something isn’t right in your patient’s current state of health. Any nurse can take these points of assessment, think critically, and save their patient from a potentially unnecessary code situation. Until next time, happy studying!
Andra Alyse